BACKGROUND:
Postoperative mediastinitis is a serious and potentially lethal complication from cardiac surgery. Although postoperative mediastinitis cannot be reliably predicted, a number of preoperative and intraoperative risk factors have been defined by previous work. The authors now present their cumulative experience with primary sternal fixation of high-risk patients as one preventative measure.
METHODS:
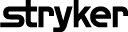
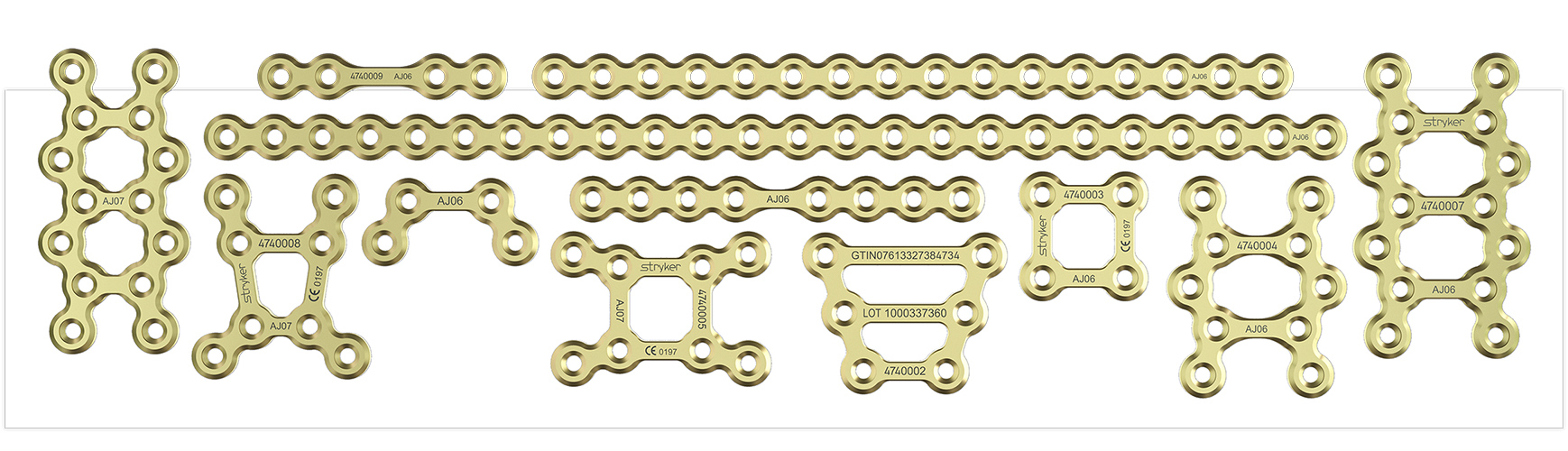
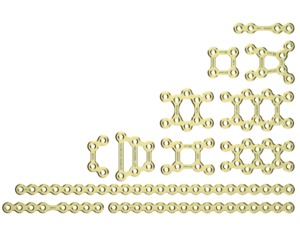
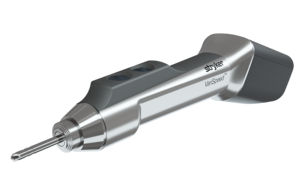
A retrospective review from July of 2000 to October of 2006 was performed on 750 patients who had at least three established risk factors for postoperative mediastinitis and received primary titanium plate sternal fixation. Patients were followed for a minimum of 6 weeks and monitored for pain, instability, wound breakdown, and plate migration.
RESULTS:
Rigid plate fixation was completed at the end of the primary cardiac surgical procedure in all 750 patients. Sternal dehiscence occurred in 18 patients (2.4 percent), necessitating reexploration. Four of these patients developed postoperative mediastinitis and had other significant comorbidities, such as ongoing inflammatory breast cancer or pneumonia, that were beyond the typical risk factors identified for developing mediastinitis. Successful sternal fixation was therefore accomplished in 732 patients (97.6 percent). Despite changes in instrumentation and technique, this approach was adopted by the cardiac surgical team consistently after an initial mentoring and training period by the plastic surgeons.
CONCLUSIONS:
Primary sternal fixation is a simple and reliable method for prevention of postoperative mediastinitis development in high-risk patients. This technique, conceptualized by plastic surgeons, is now being implemented by cardiac surgeons in increasing numbers. This demonstrates the ability for plastic surgery to initiate a paradigm shift in other fields of medicine and to decrease the complications that primarily affect our practice.


.jpg)




