HydroSet
Overview
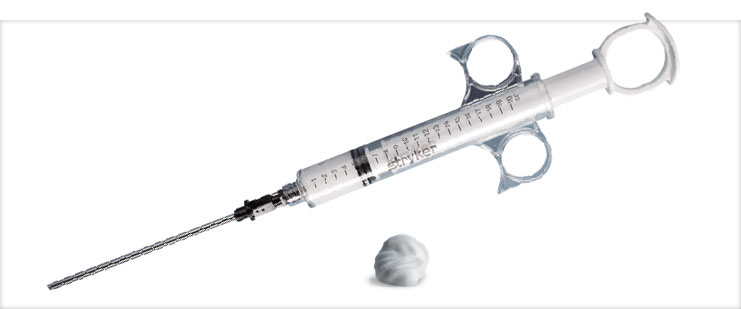
HydroSet is a self-setting, calcium phosphate cement intended for use in the repair of neurosurgical burr holes, contiguous craniotomy cuts and other cranial defects as well as in the augmentation or restoration of bony contour in the craniofacial skeleton.
The standard in HA cement.
Features and benefits
Wet field characteristics
HydroSet is formulated to harden in the presence of water, blood, and CSF, which allows for irrigation/ wash out of the surgery site during setting.2,3
Fast setting
HydroSet has been specifically designed to set quickly once implanted under normal physiological conditions, potentially minimizing procedure time.1
Osteoconductive
HydroSet is a calcium phosphate cement that hardens to form hydroxyapatite and remodels to natural bone through osteoclastic resorption and new bone formation.1
Isothermic
HydroSet avoids thermal injury as it does not give off any potentially damaging heat as it hardens.1
Clinical evidence
OBJECT
Calcium phosphate cement provides a biomaterial that can be used for calvarial reconstruction in a retrosigmoid craniectomy formicrovascular decompression (MVD). This study evaluates the outcomes of postoperative CSF leak and wound infection for patients undergoing acomplete cranioplasty using calcium phosphate cement versus incomplete cranioplasty using polyethylene titanium mesh following a retrosigmoid craniectomy for MVD.
METHODS
The authors evaluated 211 cases involving patients who underwent first-time retrosigmoid craniectomiesperformed by a single attending surgeon fortrigeminal neuralgia from October 2008 to June 2014. From this patient population, 111 patients underwent calvarial reconstruction after retrosigmoid craniectomy using polyethylene titanium mesh, and 100 patients had reconstructions usingcalcium phosphate cement. A Pearson's chi-square test was used to compare postoperative complications of CSF leak and wound infection in these 2 types of cranioplasties.
RESULTS
The polyethylene titanium mesh group included 5 patients (4.5%) with postoperative CSF leak or pseudomeningocele and 3 patients (2.7%) with wound infections. In the calcium phosphate cement group, no patients had a CSF leak, and 2 patients (2%) had wound infections. This represented a statistically significant reduction of postoperative CSF leak in patients who underwentcalcium phosphate reconstructions of their calvarial defect compared with those who underwent polyethylene titanium mesh reconstructions (p = 0.03). No significant difference was seen between the 2 groups in the number of patients with postoperative wound infections.
CONCLUSIONS
Calcium phosphate cement provides a viable alternative biomaterial for calvarial reconstruction of retrosigmoid craniectomy defects in patients who have an MVD. The application of this material provides a biocompatible barrier that reduces the incidence of postoperative CSF leaks.
OBJECTIVE
To update the outcome of hydroxyapatite cement cranioplasty in translabyrinthine acoustic neuroma (TLAN) surgery.
PATIENTS
One hundred eight previously reported patients undergoing abdominal fat graft reconstruction versus hydroxyapatite cement cranioplastywith additional 4-year follow up. Ninety additional patients undergoing a uniform technique of hydroxyapatite cement cranioplasty after TLAN.
INTERVENTION(S)
After TLAN, strips of abdominal fat are placed through the dural opening and medial to the level of the mastoid antrum, filling the lateral mastoid cavity.
MAIN OUTCOME MEASURE(S)
Cerebrospinal fluid (CSF) leaks and wound complications.
RESULTS
No additional CSF leaks or wound complications were identified in the patients included in the previous report. In the new series of 90 consecutive patients, there was one CSF leak.
CONCLUSION
Hydroxyapatite cranioplasty is a reliable method to avoid CSF leaks after TLAN surgery.
OBJECT
Several prophylactic surgical methods have been tried to prevent CSF leakage after translabyrinthine resection of acoustic neuroma(TLAN). The authors report an improvised technique for multilayer watertight closure using titanium mesh-hydroxyapatite cement (HAC) cranioplastyin addition to dural substitute and abdominal fat graft after TLAN.
METHODS
The study was limited to 42 patients who underwent TLAN at University Hospitals Case Medical Center using this new technique from 2006 to 2012. Systematic closure of the surgical wound in layers using temporalis fascia, dural substitute, dural sealant, adipose graft, titaniummesh, and then HAC was performed in each case. Temporalis muscle and eustachian tube obliteration were not used. The main variables studied were patient age, tumor size, tumor location, cosmetic outcome, length of hospitalization, and the incidence of CSF leak, pseudomeningocele, and infection.
RESULTS
Excellent cosmetic outcome was achieved in all patients. There were no cases of postoperative CSF rhinorrhea, incisional CSF leak, or meningitis. Cosmetic results were comparable to those achieved using HAC alone. This cost-effective technique used only a third of the HAC required for traditional closure in which the entire mastoid defect is filled with cement, predisposing to infection. Postoperative CT and MRI showed excellent bony contouring and dural reconstitution, respectively.
CONCLUSIONS
The authors report on successful use of titanium mesh-HAC cranioplasty in preventing postoperative CSF leak after TLAN in all cases in their series. The titanium mesh provides a well-defined anatomical dissection plane that would make reoperation easier than working through scarred soft tissue. The mesh bolsters the fat graft and keeps HAC out of direct contact with mastoid air cells, thereby reducing the risk of infection. The cement cranioplasty does not preclude subsequent implantation of a bone-anchored hearing aid.
The search for a universal reconstructive material and the application of a routine approach leaves the surgeon limited in cranial reconstruction. Facility with a variety of implant materials and approaches helps optimize surgical management. The variability of surgical defects and challenges incranial reconstruction highlights the importance of a strategic approach to evaluate both the defect and the clinical circumstance. Among the numerous alloplastic materials available, the utility of titanium mesh, hydroxyapatite cement, and prefabricated custom acrylic implants have remained at the forefront. The onus of responsibility remains on the surgeon to evaluate each clinical scenario and select the optimal course for management.
BACKGROUND
Following retromastoid craniectomy for microvascular decompression of the fifth or seventh cranial nerve, the preferred method and value of cranioplasty remains disputed.
METHODS
In this study, we report the functional outcome of calcium phosphate cranioplasty following first-time microvascular decompression in 79 consecutive patients who underwent operations over a one-year period.
RESULTS
No patient experienced a deep infection, cerebrospinal fluid leak or undue incisional pain at long-term follow-up. Additionally, all patients stated that they were satisfied with the cosmetic outcome.
DISCUSSION
Although this technique is unlikely to affect the rates of infection and postoperative pain, we believe that the low rate of CSF leak provides a unique advantage over other currently used methods of closing retromastoid craniectomies.
We report a novel technique for closure using titanium mesh cranioplasty in addition to hydroxyapatite cement and abdominal fat graft for acoustic neuroma. We reviewed 15 patients who underwent translabyrinthine craniectomy for resection of acoustic neuroma. Hearing loss was documented prior to surgical procedure. Over 2 years, patients underwent titanium mesh and hydroxyapatite cranioplasty with abdominal fat graft. Participants included seven men and eight women, age range 38 to 65. Main outcome measures included cosmetic outcome and incidence of cerebrospinal fluid (CSF) leak. The lesion was right-sided in seven patients and left-sided in eight. Cosmetic outcome was excellent in all. There were no cases of CSF leak. Closure used one-third the hydroxyapatite required for traditional closure. Our technique yields cosmetic results equivalent to hydroxyapatite cement alone and a comparable incidence of CSF leakage without leaving a drain in place postoperatively. The technique is easy to adopt, is more cost-effective than hydroxyapatite cement cranioplasty alone, offers greater ease of access for reoperation, and does not preclude later implantation of bone-anchored hearing aid.
References:
1. Larsson, S.: Injectable Phosphate Cements – A Review. 2006.
2.Hannink, G., Wolke, J.G.C., Schreurs, B.W., Buma, P.: In Vivo Behavior of a Novel Injectable Calcium Phosphate Cement Compared with
Two Other Commercially Available Calcium Phosphate Cements. 2007.
3.HydroSet IFU
CMF-WC_48_Rev. None_18987