Overview
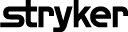
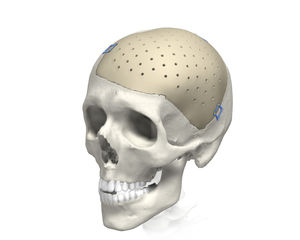
Cranial iD implants allow you to address your patients desire for complete restoration and aesthetic results that are available in the material of your choice including MEDPOR (porous polyethylene) and PEEK (Poly-Ether-Ether-Ketone). Each implant is uniquely designed to fit the bony void and individual anthropometry of your patient. Your input drives the artistry of each implant through a design session with a Stryker Design Engineer who takes your input and customizes an implant with exceptional anatomical fit and contour that is designed for an excellent post-operative patient experience.
Material option features and benefits:
 PEEK
PEEK
PEEK customized implants by Stryker are designed with exacting parameters to optimize the bone-to implant interface. Multiple fit options are available to accommodate the needs of both you and your patient.
PEEK CCI has a longstanding proven history with an excellent safety profile fully supported by documented clinical evidence. The “best in class” support and expertise of your local Stryker representative combined with the strength and fit of your implant allow you to close and reconstruct with confidence.
Available in PEEK Priority (no design session) and PEEK Complex (requires design session).
Clinical evidence
Craniectomy defects following resection of calvarial lesions are most often reconstructed using on-table manufacturing. With the advent of computer-aided design/manufacturing and customized craniofacial implants (CCIs), there seems to be more suited alternatives. In this study, the authors report their institutional experience and outcome using immediate, single-stage, CCI-based reconstruction for benign and malignant skull neoplasm defects.
METHODS
A retrospective review of a prospectively maintained database of all implant cranioplasties performed between 2011 and 2014, by a single craniofacial surgeon at a tertiary academic medical institution was performed. Preoperative and postoperative computed tomography scans with 3D reconstruction were performed for the purpose of assessing adequate resection and reconstructive outcomes. Primary endpoints included length of surgery, predicted defect versus postoperative implant surface area, contour irregularities, and complications.
RESULTS
Of the 108 patients with cranioplasty identified, 7 patients were found to undergo immediate CCI-based reconstruction for calvarialneoplasms; 4 patients (4/7, 57%) presented with malignant pathology. All defects were >5 cm2. As compared with their original size, all implantswere modified intraoperatively between 0.2% and 40.8%, with a mean of 13.8%. With follow-up ranging between 1 and 16 months, there were no implant-related complications identified. The immediate and long-term aesthetic results, as well as patient satisfaction, were ideal.
CONCLUSION
With this preliminary experience, the authors have successfully demonstrated that immediate customized implant reconstructive techniques, by way of intraoperative modification, are both safe and feasible for benign and malignant skull neoplasms. The authors believe that with wider acceptance of this multidisciplinary approach and increased surgeon familiarity, this technique will soon become the reconstructive standard of care.
BACKGROUND
Although materials for secondary cranial reconstruction have evolved with time, the overall approach in terms of bone flap/implantreconstruction after necessary delay has remained constant.
OBJECTIVE
To present our cases series of 50 consecutive secondary cranial reconstruction patients and to describe a multidisciplinarycranioplasty approach developed to reduce morbidity, to minimize infection, and to improve aesthetic appearance.
METHODS
Standard technique teaches us to place the bone flap and/or alloplastic implant directly over the dura or dural protectant after scalp flap re-elevation. However, this procedure is fraught with high complication rates, including infection. While raising the previously incised scalp flap overlying the full-thickness calvarial defect, the dissection is performed within the loose areolar tissue plane beneath the galea aponeurosis, thus leaving vascularized pericranium intact over the dura.
RESULTS
A total of 50 consecutive patients were treated by the senior author encompassing 46 cranioplasties using the pericranial-onlayapproach, along with 4 isolated temporal soft tissue reconstructions with liquid poly-methyl-methacrylate. Of the 46 cranioplasties (> 5 cm), only 1 autologous bone flap developed deep infection necessitating bone flap removal (1 of 46, 2.17%; 95% confidence interval, 0.003-11.3). None of the alloplastic custom implants placed have developed any infection requiring removal.
CONCLUSION
This multidisciplinary approach illustrated in our case series, including our "pericranial-onlay" technique described here for the first time, has the potential to improve patient outcomes, to decrease perioperative morbidity, and to minimize costs associated with postoperative infections after secondary cranial reconstruction.
Pterional PLUS
MEDPOR
MEDPOR is a biocompatible, porous polyethylene material. The interconnecting, omni-directional pore structure may allow for fibro vascular in-growth and integration of the patient’s tissue. The material of this implant makes it easy to modify with a burr or scalpel.
Clinical evidence

Craniectomy defects following resection of calvarial lesions are most often reconstructed using on-table manufacturing. With the advent of computer-aided design/manufacturing and customized craniofacial implants (CCIs), there seems to be more suited alternatives. In this study, the authors report their institutional experience and outcome using immediate, single-stage, CCI-based reconstruction for benign and malignant skull neoplasm defects.
METHODS
A retrospective review of a prospectively maintained database of all implant cranioplasties performed between 2011 and 2014, by a single craniofacial surgeon at a tertiary academic medical institution was performed. Preoperative and postoperative computed tomography scans with 3D reconstruction were performed for the purpose of assessing adequate resection and reconstructive outcomes. Primary endpoints included length of surgery, predicted defect versus postoperative implant surface area, contour irregularities, and complications.
RESULTS
Of the 108 patients with cranioplasty identified, 7 patients were found to undergo immediate CCI-based reconstruction for calvarialneoplasms; 4 patients (4/7, 57%) presented with malignant pathology. All defects were >5 cm2. As compared with their original size, all implantswere modified intraoperatively between 0.2% and 40.8%, with a mean of 13.8%. With follow-up ranging between 1 and 16 months, there were no implant-related complications identified. The immediate and long-term aesthetic results, as well as patient satisfaction, were ideal.
CONCLUSION
With this preliminary experience, the authors have successfully demonstrated that immediate customized implant reconstructive techniques, by way of intraoperative modification, are both safe and feasible for benign and malignant skull neoplasms. The authors believe that with wider acceptance of this multidisciplinary approach and increased surgeon familiarity, this technique will soon become the reconstructive standard of care.
BACKGROUND
Although materials for secondary cranial reconstruction have evolved with time, the overall approach in terms of bone flap/implantreconstruction after necessary delay has remained constant.
OBJECTIVE
To present our cases series of 50 consecutive secondary cranial reconstruction patients and to describe a multidisciplinarycranioplasty approach developed to reduce morbidity, to minimize infection, and to improve aesthetic appearance.
METHODS
Standard technique teaches us to place the bone flap and/or alloplastic implant directly over the dura or dural protectant after scalp flap re-elevation. However, this procedure is fraught with high complication rates, including infection. While raising the previously incised scalp flap overlying the full-thickness calvarial defect, the dissection is performed within the loose areolar tissue plane beneath the galea aponeurosis, thus leaving vascularized pericranium intact over the dura.
RESULTS
A total of 50 consecutive patients were treated by the senior author encompassing 46 cranioplasties using the pericranial-onlayapproach, along with 4 isolated temporal soft tissue reconstructions with liquid poly-methyl-methacrylate. Of the 46 cranioplasties (> 5 cm), only 1 autologous bone flap developed deep infection necessitating bone flap removal (1 of 46, 2.17%; 95% confidence interval, 0.003-11.3). None of the alloplastic custom implants placed have developed any infection requiring removal.
CONCLUSION
This multidisciplinary approach illustrated in our case series, including our "pericranial-onlay" technique described here for the first time, has the potential to improve patient outcomes, to decrease perioperative morbidity, and to minimize costs associated with postoperative infections after secondary cranial reconstruction.