PEEK Customized Implant
Overview
Stryker CMF PEEK Customized Implants are designed individually for each patient to replace bony voids in the cranial and craniofacial skeleton. PEEK implants may provide a strong, rigid reconstruction along with excellent anatomical fit and contour.
Precise fit. Excellent strength.
Features and benefits
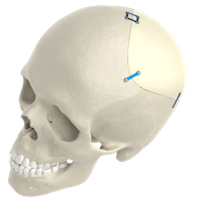
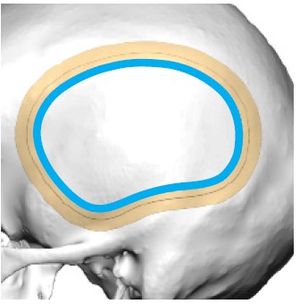
Precise fit
Designed and manufactured to product a “drop-in” fit.
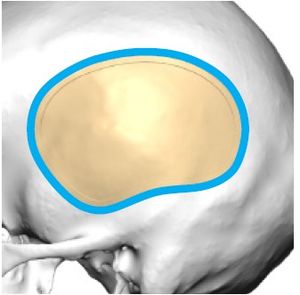
Thickness options
Implant wall thickness provided in either 3.3mm, 4mm, 5mm, or 6mm to cater patient-specific needs.
Host bone
Provided standard in each implant kit, providing a pre-operative guide to demonstrate fit.
Strong
115 Mpa Yield Strength.
PEEK Single Stage
PEEK Single Stage allows the surgeon to address their patients’ needs in one surgery. Through pre-surgical planning a predictive craniotomy is made, leading to the design of a patient-specific implant delivered to the hospital prior to surgery.
Surgeon collaboration will be required at the design phase to best identify the important inputs needed for design which include the following:
- Define resection plan and design PEEK implant
- Anatomical landmarks and CT reference points
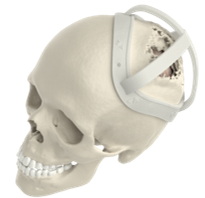
3D Systems VSP® solutions
For PEEK Single Stage cases, 3D Systems offers surgical marking guides and anatomical models to assist with the craniotomy. Marking guides are available in either a cap or ring style.
Navigation
Navigation can be integrated into PEEK Single Stage cases. Transfer the planned resection outline to the patient’s bony anatomy using compatible navigation system (STL and DICOM files).

Clinical evidence
Craniectomy defects following resection of calvarial lesions are most often reconstructed using on-table manufacturing. With the advent of computer-aided design/manufacturing and customized craniofacial implants (CCIs), there seems to be more suited alternatives. In this study, the authors report their institutional experience and outcome using immediate, single-stage, CCI-based reconstruction for benign and malignant skull neoplasm defects.
METHODS
A retrospective review of a prospectively maintained database of all implant cranioplasties performed between 2011 and 2014, by a single craniofacial surgeon at a tertiary academic medical institution was performed. Preoperative and postoperative computed tomography scans with 3D reconstruction were performed for the purpose of assessing adequate resection and reconstructive outcomes. Primary endpoints included length of surgery, predicted defect versus postoperative implant surface area, contour irregularities, and complications.
RESULTS
Of the 108 patients with cranioplasty identified, 7 patients were found to undergo immediate CCI-based reconstruction for calvarialneoplasms; 4 patients (4/7, 57%) presented with malignant pathology. All defects were >5 cm2. As compared with their original size, all implantswere modified intraoperatively between 0.2% and 40.8%, with a mean of 13.8%. With follow-up ranging between 1 and 16 months, there were no implant-related complications identified. The immediate and long-term aesthetic results, as well as patient satisfaction, were ideal.
CONCLUSION
With this preliminary experience, the authors have successfully demonstrated that immediate customized implant reconstructive techniques, by way of intraoperative modification, are both safe and feasible for benign and malignant skull neoplasms. The authors believe that with wider acceptance of this multidisciplinary approach and increased surgeon familiarity, this technique will soon become the reconstructive standard of care.
BACKGROUND
Although materials for secondary cranial reconstruction have evolved with time, the overall approach in terms of bone flap/implantreconstruction after necessary delay has remained constant.
OBJECTIVE
To present our cases series of 50 consecutive secondary cranial reconstruction patients and to describe a multidisciplinarycranioplasty approach developed to reduce morbidity, to minimize infection, and to improve aesthetic appearance.
METHODS
Standard technique teaches us to place the bone flap and/or alloplastic implant directly over the dura or dural protectant after scalp flap re-elevation. However, this procedure is fraught with high complication rates, including infection. While raising the previously incised scalp flap overlying the full-thickness calvarial defect, the dissection is performed within the loose areolar tissue plane beneath the galea aponeurosis, thus leaving vascularized pericranium intact over the dura.
RESULTS
A total of 50 consecutive patients were treated by the senior author encompassing 46 cranioplasties using the pericranial-onlayapproach, along with 4 isolated temporal soft tissue reconstructions with liquid poly-methyl-methacrylate. Of the 46 cranioplasties (> 5 cm), only 1 autologous bone flap developed deep infection necessitating bone flap removal (1 of 46, 2.17%; 95% confidence interval, 0.003-11.3). None of the alloplastic custom implants placed have developed any infection requiring removal.
CONCLUSION
This multidisciplinary approach illustrated in our case series, including our "pericranial-onlay" technique described here for the first time, has the potential to improve patient outcomes, to decrease perioperative morbidity, and to minimize costs associated with postoperative infections after secondary cranial reconstruction.
CCI-WEB-1_Rev. None_29424