Universal Select CMF Plating
Legacy meets flexibility
Overview
The Universal Select system is a comprehensive Craniomaxillofacial titanium plating system, which includes a wide selection of high quality implants for bone fixation of Craniomaxillofacial fractures, orthognathic and reconstructive surgery.
Features and benefits
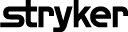
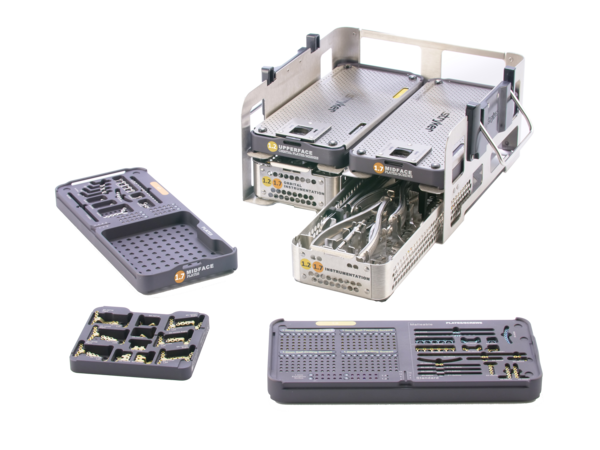
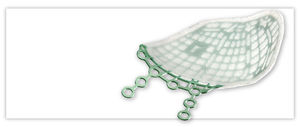
Modular design
- Implants and instruments are designed for specific anatomical regions
Enhanced customization
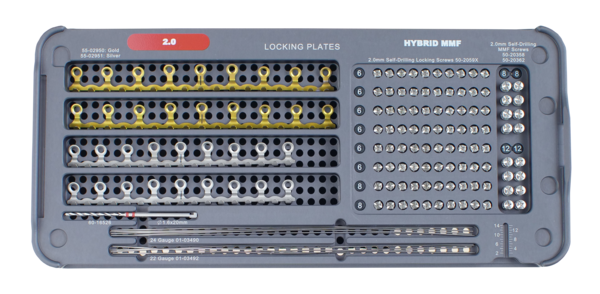
- Personalize your plating set by combining implant, instruments, and accessory trays that best fit your needs
- Utilize interchangeable inlays to easily modify plate and screw combinations
- Build unique plate pockets with silicone wall inserts
Color coding
- Labels are located on the top and sides of modules for easy identification
- Instruments have corresponding coloring to simplify use in the OR
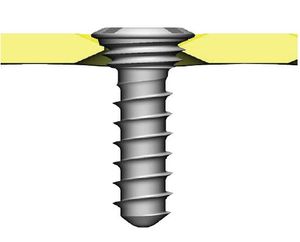
1.2/1.7mm AXS screws
- Improved off-axis stability during insertion1
- Lower profile height
- Improved screw pick-up performance1
- Improved insertion of self-drilling screws1
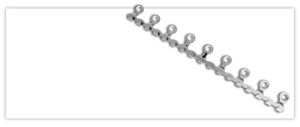
SMARTLock technology
- Creates a rigid plate to screw construct, minimizing the risk of screw backout2
- Locking capability up to 10º of angulation in every direction3
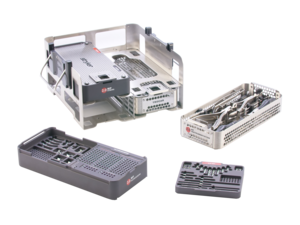
Reduced footprint
- A new, thinner design allows more plates and screws to fit in a smaller footprint
- Implant modules and instrument trays stack for simple transportation and sterilization
- Enhanced modularity allows for reduced weight
Rigid sterilization
- Racks are designed to fit into rigid sterilization containers to eliminate the need for blue wrap
Clinical evidence
PURPOSE
Three-dimensional imaging using digital volume tomography after reduction of zygomaticomaxillary complex fractures was performed and evaluated.
PATIENTS AND METHODS
Ten patients admitted for surgical treatment of zygomaticomaxillary complex fractures were included in the study. All patients were male, aged 17 to 81 years (average, 43.8 years). Preoperative diagnostics and surgical treatment involving open reduction under general anesthesia were performed as usual. One to 3 days (average, 1.6 days) postoperatively, a digital volume tomography data set was generated using the NewTom 9000 (NIM s.r.l., Verona, Italy). After DICOM-import in eFilm Workstation 1.8.3 (Merge Technologies Inc, Milwaukee, WI), axial, coronal, and sagittal reconstructions were evaluated by 6 examiners with the help of 5 defined criteria.
RESULTS
One data set was sufficient to visualize all fracture sites of the midface in all patients. Postprocessing using eFilm was successfully performed in all cases. Best scoring results were found regarding bony anchorage of screws and fitting of plates. Remarkable was the low level of metal artifacts in primary and secondary reconstructions, even in close proximity of the material. Most difficulty was encountered during the identification of the medial orbital wall, especially next to poorly ventilated ethmoidal cells. Osseous structures of older patients with decreased bone density proved difficult to visualize.
CONCLUSION
Digital volume tomography using the NewTom 9000 is suitable for assessment of postoperative results after zygomaticomaxillary complex reduction.
This prospective randomized clinical trial compared the treatment outcomes of strut plate and Champy miniplate in fixation of mandibular angle fractures. Patients with mandibular angle fracture were consented and enrolled into this study. Exclusion criteria include patients with severely comminuted fractures. The patients were randomly assigned to receive the strut plate or Champy miniplate for angle fracture fixation. Patient demographics, fracture characteristics, operative and postoperative outcomes were collected prospectively. Statistical analysis was performed to evaluate the significance of the outcome. A total of 18 patients were included in this study and randomly assigned to receive either the strut plate or Champy miniplate. Out of which five patients were excluded postoperatively due to complex fracture resulting in postoperative maxillomandibular fixation. The final enrollment was 13 patients, N = 6 (strut) and N = 7 (Champy). There was no statistically significant difference in the pretreatment variables. Nine of these patients had other associated facial fractures, including parasymphyseal and subcondylar fractures. Most of the (11) patients had sufficient follow-up after surgery. Both groups exhibited successful clinical unions of the mandibular angle fractures. The complications associated with the mandibular angle were 20% in the strut plate group and 16.7% in the Champy group. One patient in the strut plate group had a parasymphyseal infection, requiring hardware removal. The strut plate demonstrated comparable surgical outcome as the Champy miniplate. It is a safe and effective alternative for management of mandibular angle fracture.
PURPOSE
There is very limited evaluation of the management of fractures of the bilateral mandibular angles. The purpose of this study was to determine the incidence, etiology, and outcomes of bilateral mandibular angle fractures treated with the transoral application of rigid fixation on one side and nonrigid fixation on the other.
PATIENTS AND METHODS
Patients 18 years of age or older with isolated, noncomminuted fractures through the right and left mandibular angles and treated solely with 2.0-mm miniplates through intraoral incisions (and trocar) were collected from 2 sources. Patients treated at Allegheny General Hospital (Pittsburgh, PA) were prospectively collected from August 1, 2006 through December 31, 2012. Patients treated at Parkland Memorial Hospital (Dallas, TX) and University Hospital in San Antonio (San Antonio, TX) from January 1, 1992 through December 31, 2012 were retrospectively added to the sample. Data collected included age, gender, race, cause of fracture, presence or absence of mandibular third molars, occlusal relation documented at last visit, and occurrence and management of complications. Standard descriptive statistics were used and the relation between initial displacement and adequacy of reduction was evaluated with the Fisher exact test.
RESULTS
Of 1,565 patients with 2,195 mandibular fractures, 33 (2.1%) presented with bilateral mandibular angle fractures. The average age of the cohort was 25.2 ± 1.8 years (range, 18 to 48 yr). The mechanisms of injury were assaults (30 of 33, 90.9%), motor vehicle collisions (2 of 33, 6%), and a fall (1 of 33, 3%). Twenty-seven patients (81.8%) had at least 1 mandibular third molar at the time of injury. Three patients (9.1%) had minor postoperative wound problems, with 1 incident (3.0%) of malocclusion. There was no statistically significant relation between the initial displacement and the adequacy of reduction.
CONCLUSIONS
Bilateral mandibular angle fractures are a rare traumatic event that may be successfully treated with transoral rigid and nonrigid fixation with 2.0-mm miniplates.
INTRODUCTION
The objectives of this retrospective cephalometric study were to assess the amount, direction, and timing of postoperative changes after LeFort I maxillary advancement, and to identify risk factors for skeletal relapse.
METHODS
The material was selected from the files at the Department of Orthodontics, University of Oslo, and comprised 43 patients who underwent 1-piece LeFort I advancement as the only surgical procedure from 1990 to 1998. All patients were followed for 3 years by using a strict data collection protocol. Lateral cephalograms were obtained before surgery and at 5 times after surgery.
RESULTS
A mean relapse of 18% of the surgical advancement occurred. In 14% of the patients, clinically significant skeletal relapse (> or = 2 mm) was observed. Most (89%) postoperative change occurred during the first 6 months after surgery. Skeletal relapse increased significantly with degree of surgical advancement (P = .001) and degree of inferior repositioning of the anterior maxilla (P = .004) (linear regression analysis). At the end of follow-up, overjet and overbite were within clinically acceptable ranges for all patients.
CONCLUSIONS
Maxillary advancement with a 1-piece LeFort I osteotomy is a relatively stable procedure. Identified risk factors for horizontal relapse were degree of surgical advancement and degree of inferior repositioning of anterior maxilla.
References:
1. Product performance references: K231599 - Performance Testing. End User Test. AXS technology first launched in 2015 in the Universal Neuro III system. In 2019, this technology was incorporated into the SternalPlate and Upper/Mid-Face systems.
2: Knott, P.D., et al. “Evaluation of Hardware-Related Complications in Vascularized Bone Grafts with Locking Mandibular Reconstruction Plate Fixation”. Arch Otolaryngol Head Neck Surg. 2007 Dec; 133(2): 1302-6.
3: TI2124 White Paper
CMF-WC-38_Rev. None_17980